Multi-task deep learning-based radiomic nomogram for prognosis and treatment decision in nasopharyngeal carcinoma patients: a multicenter study
Please click here to the browser-based tool for CPTDN.
Induction chemotherapy (ICT) plus concurrent chemoradiotherapy (CCRT) and CCRT alone were the optional treatment regimens in locoregionally advanced nasopharyngeal carcinoma (NPC) patients. However, previous prognostic models of NPC did not take the treatment factor into account, neglecting the fact that the heterogeneity of therapy could result in their poor performances in clinical practice. We aim to use multi-task deep-learning radiomics to develop simultaneously prognostic and predictive signatures from pretreatment magnetic resonance (MR) images of NPC patients, and to construct a combined prognosis and treatment decision nomogram (CPTDN) for recommending the optimal treatment regimen and predicting the prognosis of NPC. The manuscript of this study has been submitted to the Journal of the National Cancer Institute, titled “Multi-task deep learning-based radiomic nomogram for prognosis and treatment decision in nasopharyngeal carcinoma patients: a multicenter study”.
Please click here to the browser-based tool for CPTDN.
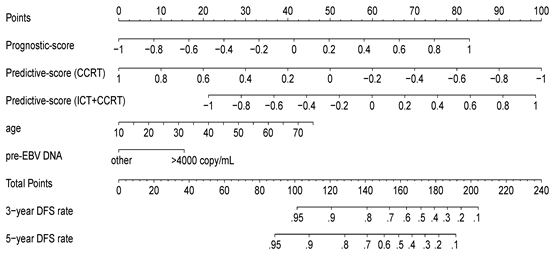
Figure 1. Combined prognosis and treatment decision nomogram (CPTDN). A CPTDN was built for predicting simultaneously disease-free survival (DFS) and treatment response. The CPTDN could noninvasively recommend an optimal treatment regimen and predict patient prognosis. For example, consider a 40-year-old target patient with stage T3N1M0, a pre-EBV DNA of >4000 copy/mL, a Prognostic-score of 0.0, and a Predictive-score of -0.4; If the patient received ICT+CCRT, the patient’s total score would be 122 (21+15+41+45), for which the 5-year DFS rate is estimated at 81%. If the patient received CCRT, the patient’s score would be 147 (21+15+41+70), for which the 5-year DFS rate is estimated at 63%. The 5-year survival benefit of receiving ICT+CCRT vs. receiving CCRT is 18%, so the CPTDN would recommend ICT+CCRT and provide a 5-year DFS rate of 81%. CCRT, concurrent chemoradiotherapy; ICT, induction chemotherapy; DFS, disease-free survival; pre-EBV DNA, pre-treatment plasma Epstein-Barr virus DNA.