A radiogenomic clinical decision support system to inform individualized treatment in advanced nasopharyngeal carcinoma
Please click here to view the model.
Both concurrent chemoradiotherapy (CCRT) and induction chemotherapy (ICT) followed by CCRT are recommended for advanced nasopharyngeal carcinoma (NPC).
However, tailoring personalized treatment is still lacking in clinical practice. Here, we established a radiogenomic clinical decision support system to classify patients into three subgroups according to their predicted survival with CCRT and ICT response, which were optimal candidates for CCRT, ICT plus CCRT, and clinical trials, respectively.
This work paves the way for precision medicine in advanced NPC and has been published at iScience, titled “A radiogenomic clinical decision support system to inform individualized treatment in advanced nasopharyngeal carcinoma”.
The browser-based tool illustrating how the proposed system aids in treatment decisions in NPC

Figure 1. The radiomics-based fusion nomogram (RFNCCRT). The RFNCCRT predicts the probability that a patient will not experience disease progression within 3 and 5 years after receiving CCRT. For example, for a patient who is newly diagnosed as stage III (T3N2M0) NPC, with the retropharyngeal lymph node (RLN) volume < 3mL and a radiomic siganture score of -0.5, the total point is about 32.5 (0+12.5+0+20) and the corresponding 3-year and 5-year DFS rates are about 89%, 85%, respectively, when receiving CCRT. NPC, nasopharyngeal carcinoma.
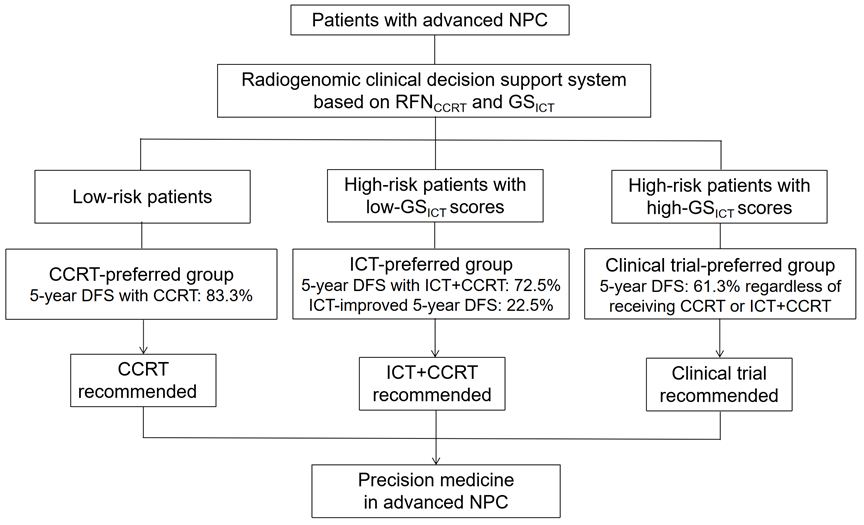
Figure 2. The schematic diagram of the radiogenomic clinical decision support system. NPC, nasopharyngeal carcinoma; RFNCCRT, radiomics-based fusion nomogram for predicting prognosis with CCRT; GSICT, 6-gene signature for predicting ICT benefit; CCRT, concurrent chemoradiotherapy; ICT, induction chemotherapy.